Human brain mapping shows neural signs of metabolic syndrome
Staff Contributor | August 14, 2019
A Texas State University professor teamed up with researchers at the Research Imaging Institute at the University of Texas Health Science Center at San Antonio to use human brain mapping data to detail neural signs of metabolic syndrome, a disease that affects nearly 35% of Americans.
Professor Larry Price, director of Methodology, Measurement and Statistical Analysis (MMSA) at Texas State, contributed to a three-prong approach that forms the foundation of “A Neural Signature of Metabolic Syndrome,” published in the August issue of Human Brain Mapping.
“We linked brain imaging information to physiological factors from our subjects,” Price said. “Then we took a third step. Through a brain map database that has 52,000 studies in it – we validated the neural signature by looking at our results and comparing it to the brain map.”
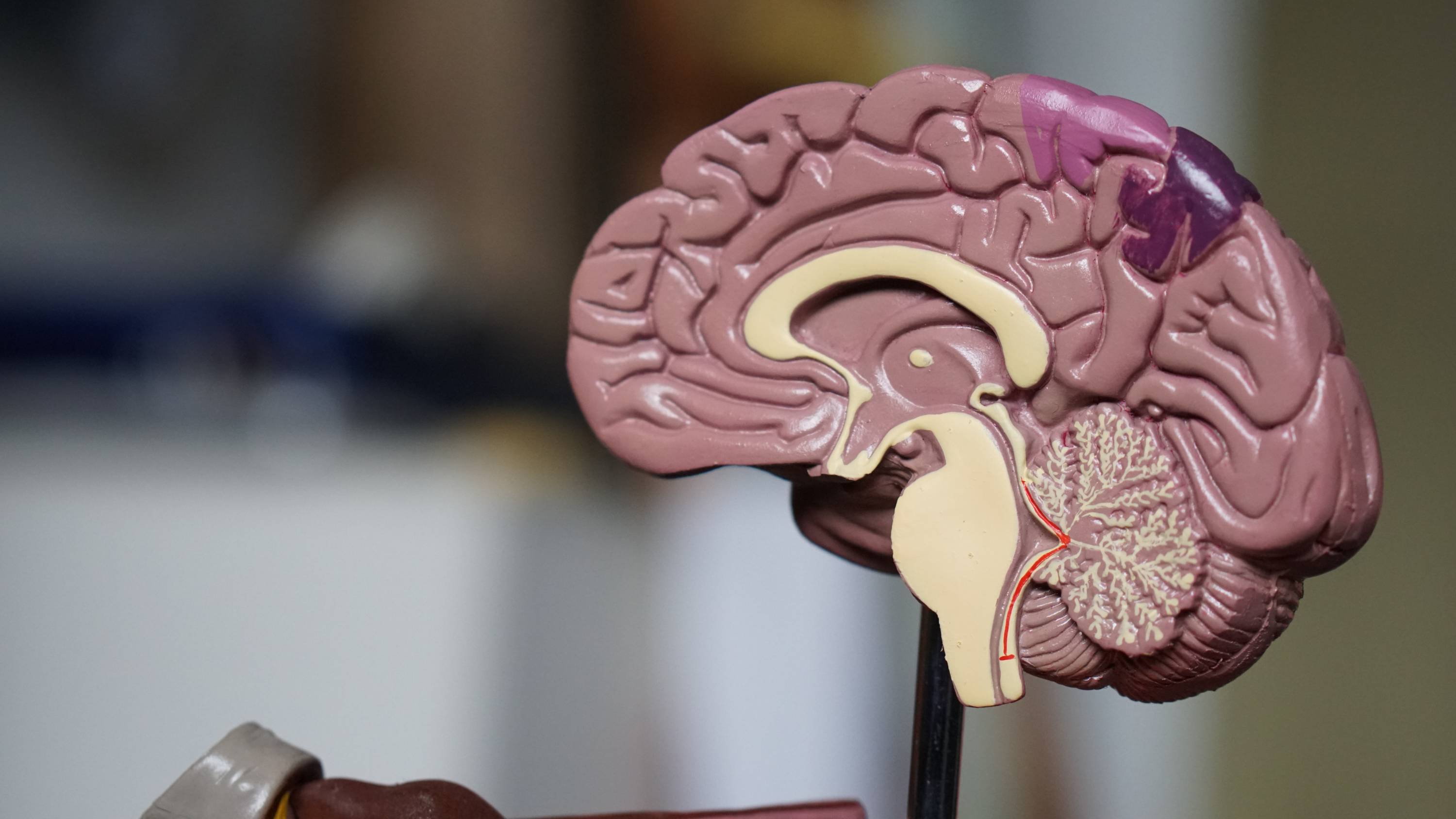
The goal: to assess how gray matter in the brain is affected by metabolic syndrome, a disease characterized by elevated blood sugar levels, increased blood pressure, reduced cholesterol and a large waistline. In a project funded by the National Institute of Mental Health, Price and the Research Imaging Institute had access to a database that focused on a group that was genetically and environmentally more at risk for metabolic syndrome: the Hispanic-American population.
“We matched that [high risk] population with a healthy control group,” Price said. “We were able to compare their metabolic syndrome variables. In that way, it was a group comparison study instead of just looking at a group that is highly susceptible to this syndrome.”
Price and his peers also examined an emerging link between metabolic syndrome and Alzheimer’s disease. That research contained a surprising element for Price.
“Not all of the regions in the brain we looked at displayed a decrease in gray matter volume in relation to previous studies that had shown that might be the case for Alzheimer’s or dementia,” Price said. “But we need to do more research on this.”
Price plans to make this data usable for healthcare providers in a clinical setting. How can they take this information about neural activity related to metabolic syndrome and help practitioners in the field?
“If you have this score on your executive function test or this score on your cholesterol test or your brain scan has certain [traits], then we can say you are more likely to develop dementia in a certain time frame,” Price said.
Share this article
For more information, contact University Communications:Jayme Blaschke, 512-245-2555 Sandy Pantlik, 512-245-2922 |